Steve Brown’s Vision for Agentic AI in Healthcare: When the Patient Is the Technologist
Steve Brown never imagined he’d be back in healthcare. Twenty years ago, he helped pioneer remote patient monitoring—long before the term became a staple in digital health conversations. He built companies, spoke at conferences, and eventually sold his business, stepping away from a field he found inspiring but exhausting. “Healthcare takes forever and is so hard to do,” he said. So he pivoted. He made films—including a celebrated documentary about Burning Man—invested in startups, and immersed himself in consumer media and entertainment.
But life had other plans.
A Diagnosis That Changed Everything
Last year, Brown began experiencing unexplained fatigue and significant weight loss. He listened to his body and, sensing something wasn’t right, underwent a comprehensive battery of tests—everything from full-body scans to blood panels and specialist consultations. The verdict? Stress, maybe gas. A fishing expedition, said one doctor.
Then fate intervened. After the Palisades fire destroyed his home and displaced him to Palm Desert, Brown ended up in a local emergency room after a steak dinner gone wrong. With no prior records or biases attached to his name, the ER team re-evaluated his symptoms—and pieced together what others had missed.
The diagnosis: a rare form of multiple myeloma, a type of blood cancer.
Suddenly, Brown found himself on the other side of the healthcare system—not as a technologist or entrepreneur, but as a patient navigating uncertainty, fear, and the need for answers. “I was back in the hospital,” he recalled, “but this time on the other side of the camera.”
What If AI Had Caught It First?
Brown had a new question: “When would AI have found this?”
He’d spent the last few years working deeply in artificial intelligence, building tools in media and education. Now, as a patient, he wanted to know if the very same technology he’d been building elsewhere could have helped diagnose him sooner—or at least make sense of the overwhelming flow of medical data.
So he built it.
Using the exact same data from his earlier lab results—the ones dismissed as inconclusive—Brown created a scenario to test AI's diagnostic capabilities. He fed the data into an agentic AI system he was developing and engaged with an AI agent named "Haley."
Haley didn’t hesitate.
"Your mild anemia, significantly elevated ferritin, and low immunoglobulins suggest potential bone marrow or immune system dysfunction," the agent responded. "This could explain your fatigue and weight loss. I recommend a hematology consult."
It was a startling contrast. Same data, radically different insight.
Building a Team of AI Agents
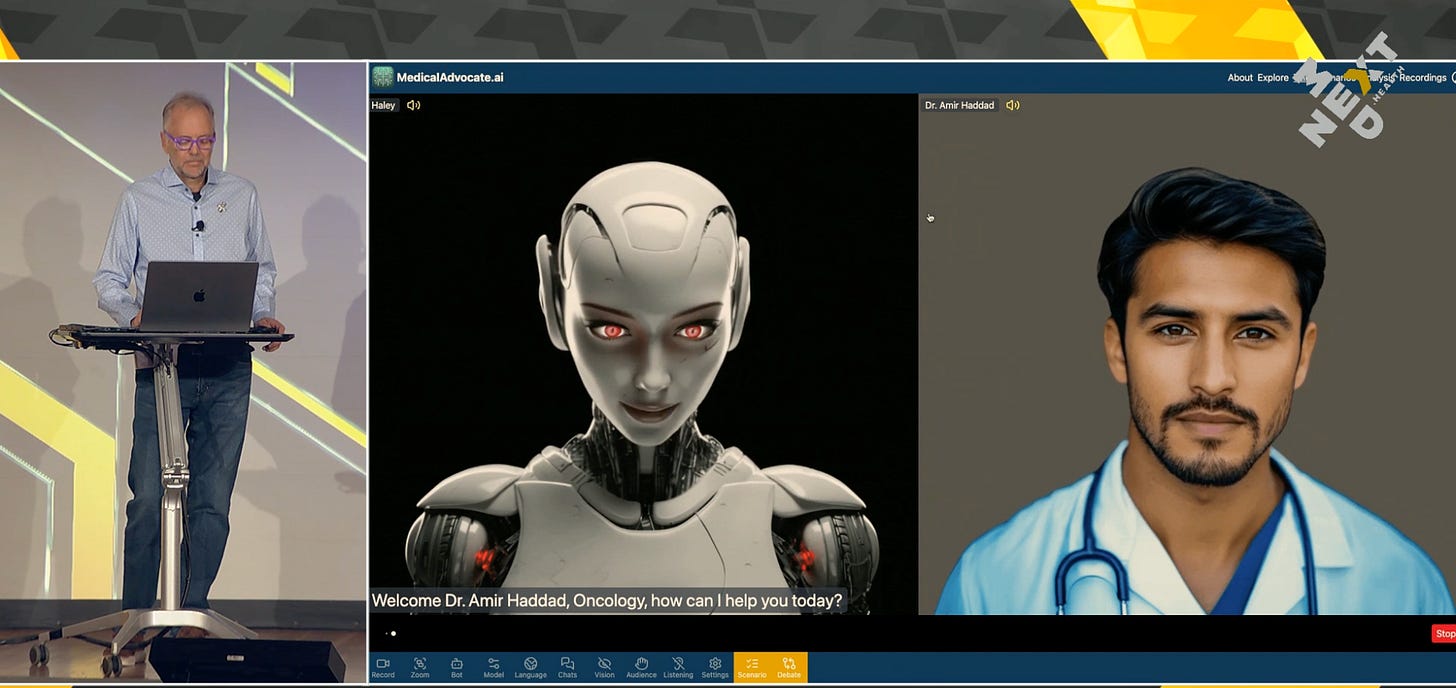
What Brown demonstrated next stunned the audience: a virtual, intelligent medical team capable of interpreting test results from different specialist perspectives. Not just one agent, but several—each with its own training and bias, just like real doctors.
There was Haley, the all-knowing generalist. Then “Dr. Amir Haddad,” an oncologist AI. Brown simulated a conversation between them, where each agent brought a different lens to the same data set—collaborating, validating, and sometimes challenging one another’s interpretations.
They converged on a key point: something was wrong in the bone marrow. A biopsy was warranted. Exactly what had been missed by the real-life specialists weeks earlier.
Then Brown scaled it.
He expanded the AI consultation to include agents simulating a cardiologist, gastroenterologist, emergency physician, and hematologist. Each parsed the same medical records, surfacing specialty-specific insights and next steps. Then he introduced "Hippocrates," an AI agent designed to serve as the synthesis layer—like a tumor board chairperson, integrating diverse perspectives into a cohesive recommendation.
This wasn’t just theoretical. It was a working prototype of what Brown calls a “swarm” of agents—intelligent collaborators who, together, help patients navigate the complexities of modern medicine with clarity, speed, and contextual relevance.
A Democratized Tumor Board
Brown wasn’t alone on stage. He introduced Lisa Booth, a longtime friend and metastatic breast cancer “thriver” who had navigated her own high-stakes care journey over the past decade.
Booth, a veteran of multiple clinical trials, described how she had built an informal network of specialists and advocates to guide her treatment decisions—including an interventional radiologist neighbor and a friend who helped bring CAR-T therapy through the FDA.
Even with access most patients could only dream of, Booth said, coordinating care between specialists remained her responsibility. “My oncologist is amazing, but she doesn’t have time to coordinate everything,” she noted. “When it comes to local treatment, I became the quarterback.”
Working with Brown, she fed her real-world diagnostic and treatment data into his agentic AI platform. What emerged was a virtual version of her tumor board—complete with an oncologist, radiation oncologist, interventional radiologist, and surgeon. Each agent reviewed her data, weighed in, and made treatment recommendations. Then the "chairperson" agent synthesized everything into a clear path forward.
“I got better answers today than I did 18 months ago,” Booth said. “And I didn’t have to fly to Seattle, book multiple appointments, and wait weeks for follow-ups.”
Not a Replacement—An Empowerment Tool
Brown was quick to clarify: “This doesn’t replace your doctor. It makes your relationship with your doctor better.” Patients equipped with intelligent agents can ask more informed questions, better understand their options, and avoid being overwhelmed or dismissed.
Booth agreed. “It helps me have a better conversation with my oncologist,” she said. “It empowers me—but it also helps me drive them a little nuts, in a good way.”
This sentiment sparked laughter from the audience—but also raised a serious point. Many clinicians worry about AI tools encouraging “Google patient syndrome,” where misinformation leads to conflict. Brown acknowledged this tension, noting that it’s already happening with large language models like ChatGPT.
“The question isn’t whether patients will use AI,” he said. “It’s how we help them use it responsibly and effectively.”
To that end, Brown’s system includes tools for everything from clinical explanation to administrative support—like generating insurance appeal letters for denied treatments. “Don’t waste your oncologist’s time writing that letter,” he said. “Let AI do it.”
What’s Now, What’s Next
While the platform Brown demoed is not yet public, he hinted that it would be released in 2025. And it couldn’t come soon enough.
Each year, millions of Americans receive serious diagnoses that upend their lives. Most do not have Lisa Booth’s network or Steve Brown’s technical skills. But with agentic AI, they could have something just as powerful: a virtual support team that listens, explains, and advocates.
Brown believes this technology will be mainstream within a year. Foundational models are improving rapidly, and personalization layers—the part that tailors general medical knowledge to the individual patient—are now catching up.
“There’s a massive amount of knowledge in these models,” he said. “But it’s not just about what’s in there. It’s about how you access it, how you personalize it, and how you apply it to your specific situation.”
He envisions a future where patients can run their labs through a trusted agent, get second opinions in seconds, and enter appointments more confident and informed.
“Once you get a diagnosis, everything becomes very real, very fast,” he said. “Your doctor has 2,000 patients. You have one body—and you want to know everything.”
A New Era of Patient Power
Steve Brown’s journey—from technologist to patient to innovator—offers a profound glimpse into the next chapter of digital health. It's not about AI replacing clinicians or erasing the human element. It's about shifting power to patients, giving them tools to understand, navigate, and manage their health with unprecedented intelligence.
It’s about transforming the lonely, often opaque journey of illness into a shared, comprehensible, and empowered experience.
In the end, Brown’s talk was not just a tech demo. It was a deeply personal call to action: to build tools that don’t just impress in theory, but save lives in practice.
And to make sure that when the next patient like Steve—or Lisa—asks, “What should I do now?” there’s more than silence or guesswork.
There’s an answer.