Dr. Michael Gillam’s Vision for Scaling Breakthroughs in Healthcare: From 17 Years to One Click
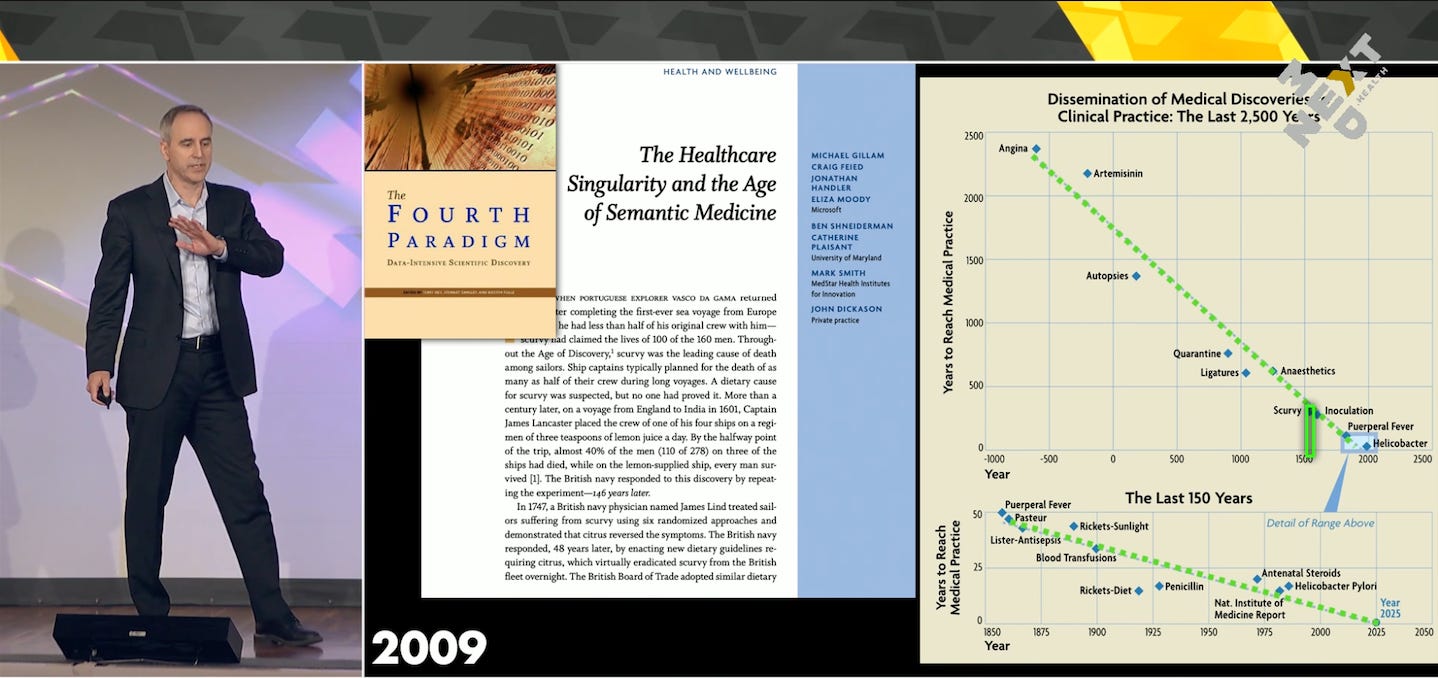
For decades, one statistic haunted healthcare innovators: it takes an average of 17 years for medical breakthroughs to reach widespread clinical adoption. Whether it’s a new treatment, a diagnostic method, or a preventative screening tool, the translation from proven science to routine care has always lagged—slow, inefficient, and obstructed by a complex web of incentives and infrastructure.
But according to Dr. Michael Gillam, physician-innovator and serial health tech entrepreneur, that’s about to change. In a stirring keynote that combined history, data science, economic theory, and real-world examples, Dr. Gillam painted a hopeful and ambitious vision for how healthcare could leap forward. The key? Harnessing exponential computational growth, building agentic systems that scale care, and rethinking both how we deliver healthcare and how we pay for it.
The Legacy of Delay: Why Good Ideas Don’t Travel Fast
Gillam opened his talk by reflecting on the familiar—but no less shocking—statistic from the Institute of Medicine: it takes 17 years, on average, for medical innovations to reach frontline care.
He gave visceral historical examples to underscore this point: it took 250 years for sailors to start carrying limes on ships after scurvy’s cure was discovered. Doctors continued to move between cadavers and delivering babies for 50 years after discovering the link to puerperal fever and the importance of handwashing.
Even today, we face a delay that’s hard to justify in the age of real-time connectivity. Innovations that could save lives linger in academic journals and pilot programs while patients suffer and die from outdated care.
But there’s a pattern in the data, Gillam said. By examining thousands of years of medical history, he and his colleagues found that the delay from innovation to adoption is converging—toward now. This decade appears poised to be a turning point, a singular moment where technology and systems align to shrink the gap between discovery and deployment.
Why Healthcare Doesn’t Prioritize Prevention
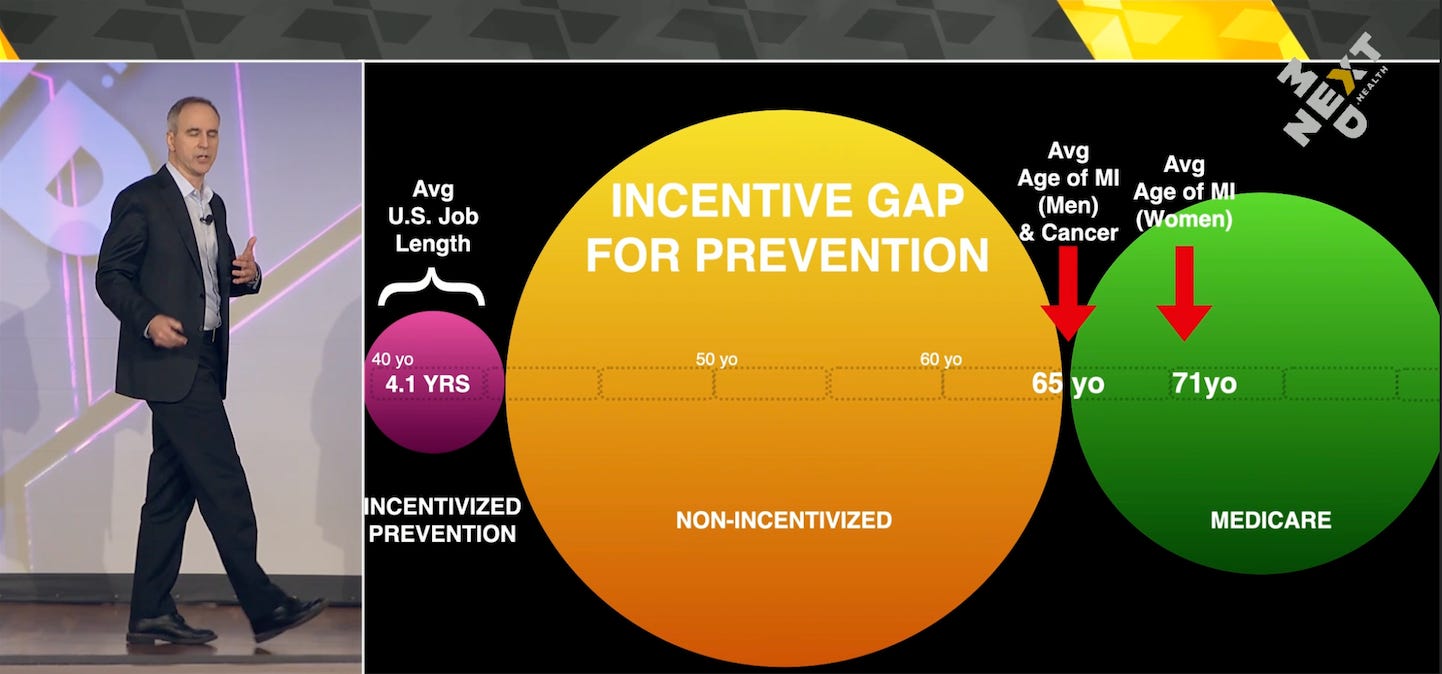
But while technological readiness is one side of the coin, Gillam emphasized that the economic structure of healthcare often works against its own stated goals.
You’ve probably heard the critique: our system focuses on “sick care,” not “well care.” But why?
Gillam provided a stark economic explanation. The average American changes jobs every 4.1 years, and each job often comes with a different insurance provider. Meanwhile, major health events—like heart attacks or cancer—often happen around age 65.
So what’s the incentive for an insurer to invest in prevention that might only pay off decades later, after the patient has switched to Medicare or another provider? From a cold cost-benefit perspective, there isn’t one. This creates a massive incentive gap where long-term health improvements are devalued—if not actively disincentivized.
To illustrate, Gillam pointed to a real-world example: an AI-enhanced heart scan that is covered 100% by insurance after age 65. But the day before your 65th birthday? It’s covered 0%. This kind of “economic step function” would be seen as absurd—and immediately arbitraged—in industries like finance or logistics. But in healthcare, it’s just Tuesday.
A Grand Challenge: Scaling the Clinician
Another challenge looms even larger: access. Some two billion people worldwide may never see a clinician in their lifetime.
“There’s no shortage of patients,” Gillam said. “What we have is a shortage of scalable care.”
He posed the grand challenge of our age: How do we scale our clinicians to impact 10x, 100x, or even 1000x more lives in a single day?
Here’s where the story turns from frustration to inspiration.
Exponential Growth in Computation: A Tidal Wave of Capability
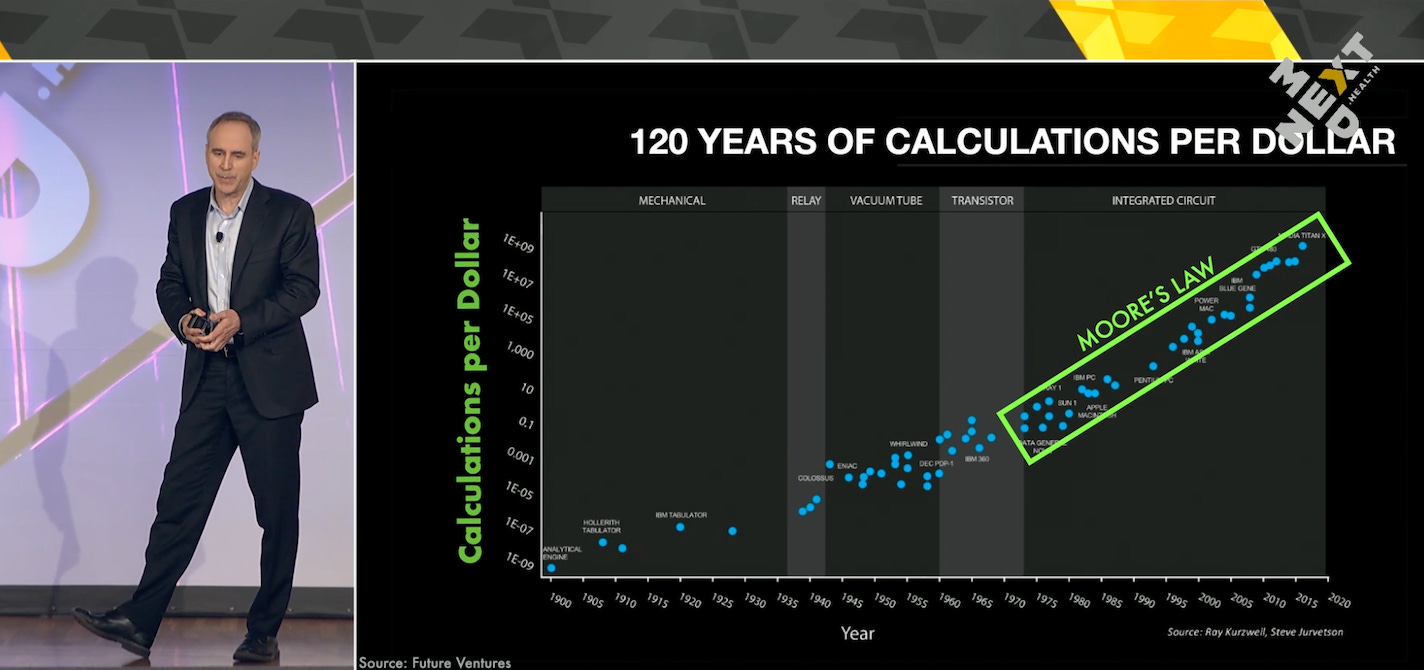
To understand what’s coming, Gillam directed the audience’s attention to a graph familiar to many technologists: the 120-year exponential growth in computing power. But he noted that most of us see it presented on a logarithmic scale, which hides the true power of the trend.
What if we visualized it as a normal graph, he asked? It becomes immediately clear: we are living through a technological explosion. Every 10 years, computers get orders of magnitude more powerful.
Gillam asked a provocative question: How soon until $1,000 can buy the computational equivalent of a human brain?
According to neuroscientists, the human brain performs about one petaflop (a quadrillion operations per second). That figure isn’t theoretical—by 2024, Nvidia had released a petaflop-class processor for under $3,000. Extrapolating the trend, future consumer devices—like the iPhone 20—will exceed the brain’s computational capacity.
“We’re moving from an internet of things,” Gillam said, “to an internet of minds.”
From Tech to Healthcare: The Age of Agentic Systems
What does this mean for healthcare?
It means that technology, when combined with AI and smart infrastructure, can help close the scale gap. One clinician supported by intelligent systems could manage thousands of patient journeys, stepping in only when necessary.
He highlighted the AI-enhanced heart scan again—this time as a microcosm of what’s possible. A 39-year-old man received the scan after being dismissed by his doctor. Labs looked fine, blood pressure was normal. But the scan revealed a dangerous “widowmaker” plaque. A stent saved his life—and he walked out able to take a deep breath for the first time in years.
That scan—augmented by AI—generated thousands of data points in minutes, work that would’ve taken a human hours. More importantly, it gave the patient a view into his own biology, and the motivation to act. He changed his diet, started biking 30 miles a day, and returned 14 months later with half the plaque he started with.
Why This Isn’t Scalable (Yet)
But Gillam also acknowledged the complexity beneath that success.
Ordering that scan, despite the AI, still requires navigating 72 logistical steps across seven sub-journeys—faxing orders, picking up CDs, verifying MD credentials. Healthcare remains a $2 trillion industry run on outdated infrastructure like fax machines and burned CDs.
To scale care, we must first scale the system that delivers it.
Enter: The Care Delivery Engine
Gillam introduced a solution: the Care Delivery Engine, a platform inspired not by hospitals but by modern e-commerce infrastructure. Think Amazon’s order tracking or Shopify’s composable commerce stack—but for health.
This engine tracks a patient’s care journey, much like Domino’s tracks a pizza. But it’s more than a tracker—it’s an orchestrator. It automates routine tasks, routes complex ones to human clinicians, and ensures that care delivery is coordinated, consistent, and proactive.
These systems allow clinicians and institutions to abstract away complexity. A patient may be on a journey that involves AI interpretation, scheduling, logistics, billing, and follow-ups—and the engine coordinates it all.
The result? A single clinician could now oversee thousands of patients on automated care pathways, jumping in only when needed to humanize the experience.
The Rise of Composable Care
Just as Amazon ushered in composable commerce, Gillam believes we’re now entering the era of “composable care.” Preventative tests, diagnostics, and health interventions become “care products” that can be bundled, tracked, and deployed at scale.
Suddenly, insurers can launch benefit storefronts, where users choose journeys like “AI Heart Scan” or “Preventative Cancer Screen.” Clinics offer health tech formularies. Even gyms and wellness centers can become access points for serious care.
Gillam cited a partner who launched what they called the “world’s first biotech bar”—the healthcare equivalent of the Apple Store’s Genius Bar. Patients could walk in, learn about diagnostics, and walk out on a guided care journey with white-glove support
Rethinking Economics: Gray Swan Pricing
To make this shift sustainable, we must rethink payment models, Gillam argued. Prevention needs better economics. He proposed a “gray swan” pricing model—flexible, data-driven pricing that attracts discretionary dollars into prevention, reducing the likelihood of catastrophic “black swan” events like heart attacks and strokes.
In such a system, scans wouldn’t be arbitrarily free at 65 and unaffordable at 64. Instead, price would vary based on risk, age, coverage, and predicted impact—just like modern pricing models in other industries.
The Marketplace Gap—and the Opportunity
Gillam closed with a quote from Andreessen Horowitz. Of the top 100 global marketplaces by GDP, at least 10 should be in healthcare. How many actually are?
Zero.
That’s the gap. And that’s the opportunity. The company—or companies—that solve this problem, that build these platforms, that make care scalable, composable, and proactive, may become the largest enterprises in history.
Conclusion: From 17 Years to One Click
Dr. Michael Gillam’s talk was a tour de force across medicine, economics, computation, and system design. But at its heart was a simple, urgent message:
Let’s not wait 17 years to save lives with proven science. Let’s build the systems that make breakthroughs usable at the point of care—immediately. Let’s turn a journey of confusion and complexity into a click.
Because with the right tools, the right economics, and the right human-AI partnership, the future of medicine isn’t 17 years away.
It’s now.